Themes > Features
09.09.2003
Does The New WTO Drugs Deal Really Benefit Developing Countries?
On 30 August 2003, just before the negotiating teams at the WTO in Geneva
went back to their respective countries to prepare for the Ministerial
Meeting at Cancun, the deadlock over intellectual property and public
health was finally broken. The TRIPs Council agreed on legal changes that
are officially supposed to make it easier for poorer countries to import
cheaper generics made under compulsory licensing if they are unable to
manufacture the medicines themselves.
The decision settled the one piece of unfinished business on intellectual
property and health that remained from the WTO Ministerial Conference in
Doha in November 2001, and which had been left hanging for the previous
months because of fierce resistance from the
US government and the multinational lobby.
The decision was
immediately hailed by some and described as a great victory for the
developing countries and indeed for the people of the world. ‘This is a
historic agreement for the WTO’, said the WTO Director-General Supachai
Panitchpakdi. ‘The final piece of the jigsaw has fallen into place,
allowing poorer countries to make full use of the flexibilities in the
WTO’s intellectual property rules in order to deal with the diseases that
ravage their people. It proves once and for all that the organization can
handle humanitarian as well as trade concerns.’
However, the actual details of the agreement suggest that such extravagant
and fulsome praise may be uncalled for. In fact, many independent
analysts, along with the NGOs and civil society groups that had been
fighting for an agreement on this issue, feel betrayed by the final
character of the resolution, and have argued that it will do little or
nothing to improve the situation for people in the developing countries in
terms of accessing cheaper life-saving drugs.
Thus, James Love of the Consumer Project on Technology has written that
‘the persons who have negotiated this agreement have given the world a new
model for explicitly endorsing protectionism.’ Oxfam and Medecin sans
Frontieres, two groups who have closely followed the negotiations, have
called the solution ‘unworkable’ saying that the ‘deal was designed to
offer comfort to the US and the western pharmaceutical industry’ and that
‘global patent rules will continue to drive up the price of medicines’.
It is even possible to argue that the final form of the resolution is
actually a step backward compared to the flexibilities that existed in the
original TRIPs agreement, and that the entrenched position of the large
international drug monopolies is further legalized by the recent
statement. However, to understand this, it is necessary to provide some
background on both the international pharmaceuticals industry, and the
TRIPs agreement and the controversies that have surrounded it.
The International Pharma Industry
Pharmaceutical markets
differ from markets for most other commodities, since drugs are rather
special commodities. Private drug markets typically suffer from a number
of forms of market failure. These include: (a) informational
imbalances—thus, for example, consumers are not in a position to judge the
quality and efficacy of drugs, which creates the need for a social
monitoring and surveillance system; (b) monopoly and lack of competition
created by patent protection, brand loyalty and market segmentation; (c)
externalities in the form of social benefits of drug consumption. Drugs
play a significant social role in that they are an integral part of the
realization of the fundamental human right to health. For these reasons,
pharmaceutical products are classified as essential goods, with the
understanding that they have to be accessible to all people.
Obviously, access to the latest available technology in this sphere is
crucially important for the health and welfare of children, not only in
terms of availability to all children but also the access of mothers.
There is clear need for some social control over investment in technology
relating to drug production, and the subsequent prices and distribution,
not only because of the market failures described above, but also since
unregulated drug markets tend to create substantial inequity, particularly
in terms of access to drugs.
The world market for drugs is a huge one, but it is dominated by only
three countries—the
United States,
Japan and Germany—which account for more than two-thirds of total sales.
In fact, only 15 per cent of the world's population accounts for 86 per
cent of drug spending, while the remaining 85 per cent get only a 14 per
cent share.
The difficulty of ensuring even a minimum degree of democratic access to
life-saving drugs is compounded by the high degree of concentration in the
international drug industry. Table 1 describes the situation in 1998, when
the top ten companies controlled 36 per cent of the market and the top
twenty companies controlled 57 per cent of world sales.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Since then there have been more mega-mergers which have made the industry
even more concentrated. Glaxo Wellcome merged with SmithKline Beecham,
Pfizer merged with Warner Lambert, and the companies Hoechst-Marion,
Merrell and Rhone-Poulenc merged to form Aventis. Currently the top ten
companies are estimated to control more than half of the world market, and
the top twenty companies more than two-thirds of the world market.
Apart from mergers, there is growing evidence that drug companies are
using the patent system to establish monopoly control. Often patents are
filed for products or chemical substances, or now even genes, whose
attributes are not fully known, simply to pre-empt the competition and
allow for monopoly rents once further research—possibly by others
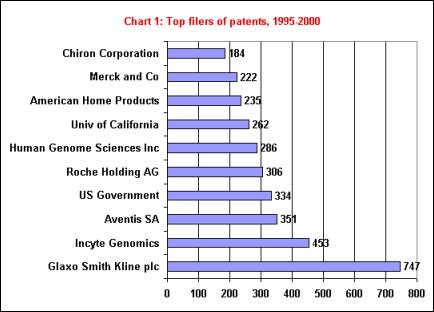
including public agencies—reveals the uses. As Table 2 shows, the top ten
filers of patents include six drug companies and two companies
specializing in genetic research.
Such monopoly allows drug companies to charge prices
that are as high as they feel the market will bear, without reference to
or well in excess of the actual costs of R&D that they may have borne.
Thus there is wide variation in prices of the same drug charged not only
by different companies but even by the same company in different markets.
As Charts 2a, 2b and 2c, show, the prices
of branded or patented products are often far higher than the prices of
similar medicines produced by alternative or generic sources.
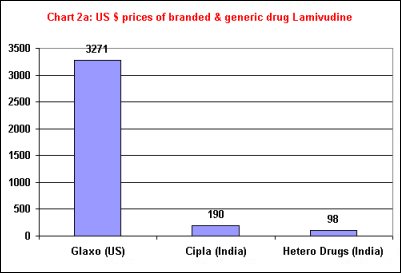
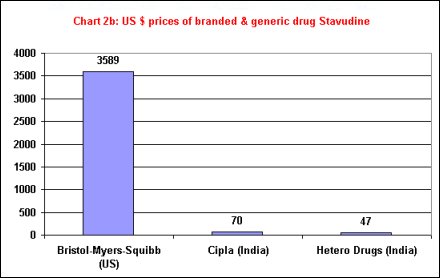
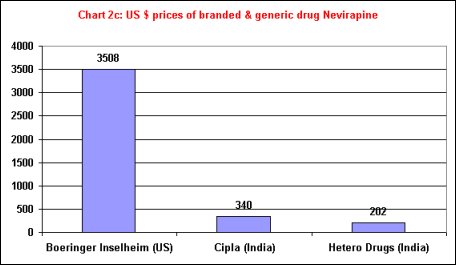
The use of market
segmentation to earn monopoly profits is obviously constrained by the
possibility of undercutting by competitors producing generic substitutes.
This possibility, and the opposition of multinational drug companies to
allowing it, was dramatically illustrated by the battle between the Indian
drug company Cipla and major MNC players over providing cheaper drugs for
AIDS patients in Africa.
The fact that
competition
from generic producers will result in the lowering and levelling of prices
of medicines is very clear even from the pricing behaviour of large
multinational drug companies in different markets. Not only do MNCs price
differently in different markets, but they tend to charge much less when
generic drug substitutes are available.
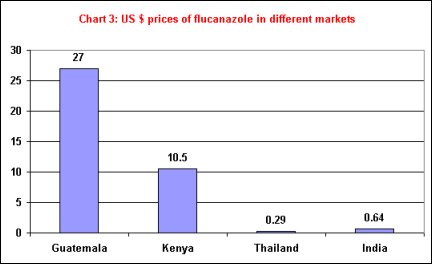
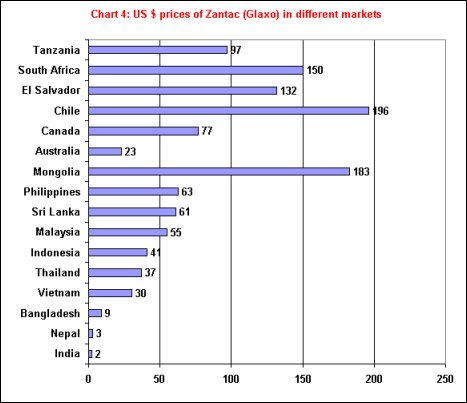
This is sharply evident
from Chart 3, which shows prices of Flucanazole in different markets, and
Chart 4, which indicates the different prices charged by Glaxo for its
anti-ulcer drug Zantac. Such pricing bears little relation to per capita
income in the country concerned, but is much more dependent upon the
existence of generic substitutes like Ranitidine, which is why the drug is
the cheapest in
India.
The TRIPS Agreement
This context explains
why there have been major concerns about the enforcement of the TRIPs
agreement, particularly with reference to health conditions in developing
countries, since the agreement is seen as increasing the power of large
corporations who may be in a position to capture patents, vis-à-vis state
regulatory authorities.
The agreement requires all WTO member states to grant patents for
pharmaceutical products or process inventions for a minimum of twenty
years. The major shift for countries like India was that the TRIPs
agreement forces upon member countries a patent regime that recognizes
product patents for chemicals and pharmaceuticals. The earlier Indian
Patent Act allowed for only process patents in these areas, which created
the possibility of reverse engineering especially for drugs, a factor that
was crucial in the rapid development of the generic drug industry in
India.
Some of the most frequently expressed concerns about the adverse
implications of TRIPs for public health include the following:
-
Increased patent protection leads to higher drug prices, while the number of patented drugs of importance from a public health point of view is likely to increase in the coming years.
-
The access gap between developed and developing countries, and between rich and poor in all countries, will continue to increase, especially as producers in developing countries have to wait for twenty years before they can have access to innovations.
-
Enforcement of the WTO regulations has an effect on local manufacturing capacity and removes a source of generic innovative quality drugs on which the poorer countries depend.
-
While technology transfer is actually to be discouraged, there are no incentives or provisions to ensure that increased revenues will go towards the development of essential medical technologies.
It is now much more widely recognized that there is no necessary correlation between socially desirable and necessary R&D in drug development, and a tight patent regime. Indeed, much of the major research in pharmaceuticals and medicine, both in the past and currently, is under the aegis of publicly funded institutions across the world. Table 2 indicates that R&D expenditure forms a relatively small part of the total revenues for large pharma companies, and is significantly less than marketing expenses. It is also worth noting that even in many western countries, pharmaceutical products remained unpatentable until the 1980s or even the 1990s, with no adverse implications for research.
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
However, even this restrictive agreement did leave
member states a certain amount of freedom in modifying their regulations.
For example, the terms
invention
and discovery
are not defined in the agreement, yet how they are defined could have
important implications, especially in the biotechnology field. The
agreement says that member states may provide limited exceptions to the
patent holder’s exclusive rights in their laws.
National public authorities may be allowed, within the conditions laid
down in the agreement, to issue compulsory licences against the patent
owner’s will when justified by the public interest. The agreement does
not prohibit parallel imports. These restore price competition for
patented products by allowing the importation (without the holder’s
consent) of identical patented products which have been manufactured for a
lower price in another country.
|
||||||||||||||||||||
Thus, compulsory licensing and parallel importing policies are two policy tools which can still play an important role in helping developing country governments make essential medicines more affordable to their citizens, although their use is being sought to be restricted by drug MNCs and their home country governments.
Compulsory Licensing
Compulsory licensing
may occur as follows: when reasons of general interest justify it,
national public authorities may allow the exploitation of a patent by a
third person without the owner’s consent. This involves a government
giving a manufacturer—which could be a company, government agency or other
party—a licence to produce a drug for which another company holds a
patent, in exchange for the payment of a reasonable royalty to the patent
holder. The effect is to introduce generic competition and drive prices
down, as has occurred in India. Compulsory licensing can lower the prices
of medicines by 75 per cent or more. Zimbabwe, for example, could issue a
license to a local company for an HIV/AIDS drug manufactured by
Bristol-Myers Squibb. The Zimbabwean firm would then manufacture the drug
for sale in Zimbabwe under a generic name, and pay a reasonable royalty to
Bristol-Myers Squibb on each sale.
Five kinds of use without authorization of the right holder are expressly
envisaged by the agreement [Correa 1999, 2000]:
-
licences for public non-commercial use by the Government;
-
licences granted to third parties authorised by the Government for public non-commercial use;
-
licences granted in conditions of emergency or extreme urgency;
-
licences granted to remedy a practice determined after administrative or judicial process to be anti-competitive;
-
licences arising from a dependent patent.
In addition, since the
agreement does not state that these are the only cases authorized, member
states are not limited in regard to the grounds on which they may decide
to grant a licence without the authorization of the patent holder. They
are in practice only limited in terms of the procedure and conditions to
be followed. Thus, in principle, compulsory licences can be issued for
considerations of public health as well as to prevent anti-competitive
practices and possible uses connected with monopoly.
Parallel Imports
Another strategy for
lowering drug prices is by parallel imports. Parallel importing involves a
government or another importer shopping in the world market for the lowest
priced version of a drug rather than accepting the price at which it is
sold in their country. In the pharmaceutical market, as has been shown,
prices tend to vary dramatically. Since parallel imports involve imports
of a product from one country and resale, without authorization of the
original seller, in another, thereby allowing the buyer to search for the
lowest world price, they can also be a tool to enable developing countries
to lower prices for consumers.
Both the promotion and the transfer of technology, as well as public
health or nutrition could justify derogation of the patentee's exclusive
rights. Scrutiny of the exceptions existing in much national legislation
gives an idea of the different possibilities [Correa, 1999]:
-
parallel importation of the protected product;
-
acts carried out on a private basis and for non-commercial purposes;
-
scientific research and experiments involving the patented invention;
-
preparation of drugs by unit and on medical prescription in pharmacy dispensaries;
-
a person being, in good faith, already in possession of the invention covered by the patent;
-
tests carried out before the expiry of the patent to establish the bio-equivalence of a generic drug.
In addition to these measures, as pointed by Correa [2000], there is scope within the TRIPs Agreement (under Article 30) for a number of exceptions to exclusive patent rights. Such exceptions must of course meet certain conditions: that is, they must be limited, they should not unreasonably conflict with the normal exploitation of the patent, and exceptions should not unreasonably prejudice the legitimate interests of the patent owner. Given these conditions, there is a wide range of exceptions that can be provided that are within the scope of Article 30, such as:
- acts done privately and/or on a non-commercial scale, or for a non-commercial purpose
- use of the invention for research
- use of the invention for teaching purposes
- experimentation for teaching purposes
- preparation of medicines under individual prescriptions
- experiments made for the purpose of seeking regulatory approval for marketing of a product after the expiry of a patent
- use of the invention by a third party that had used it bona fide before the date of application of the patent.
As can be seen, even
though the TRIPs provisions were restrictive, governments that were
anxious to ensure drug development for public health purposes could still
endeavour to push for more flexible patent regimes, if they were not
prevented from doing so by other forces. The problem was, of course, that
many developing country governments have found it difficult to implement
the more flexible provisions because of other kinds of external pressure.
The US government and other developed country governments, in particular,
because of their own large drug lobbies like phaRMa, have been
aggressively restricting governments that have or had intellectual
property rules such as compulsory licensing and parallel imports, designed
to make essential medicines more affordable to their citizens.
The Debate on TRIPS and Public Health in the WTO
This is why developing
countries were keen on explicit recognition in the WTO that public health
requirements could permit the legal implementation of loopholes that
already existed in the TRIPs document. All the subsequent activity has
been devoted to nothing more ambitious than a restatement of that basic
right.
Developing countries were essentially seeking a declaration recognizing
their right to implement certain pro-competitive measures, notably
compulsory licences and parallel imports, as needed to enhance access to
health care. They were frustrated by the opposition and pressure exerted
on some countries by the pharmaceutical industry and governments.
Moreover, some felt that the final proviso in Article 8.1 establishing
that any measures adopted,
inter alia, to protect public health should be consistent with the
provisions of the TRIPs agreement, provided
less
protection for public health than under the corresponding exceptions of
Article XX (b) of GATT and the Sanitary and Phytosanitary Measures and
Technical Barriers to Trade agreements.
TRIPs Article 8.1 states: ‘Members may, in formulating or amending their
laws and regulations, adopt measures necessary to protect public health
and nutrition, and to promote the public interest in sectors of vital
importance to their socio-economic and technological development, provided
that such measures are consistent with the provisions of this Agreement.’
The GATT Article XX: ‘Nothing in this Agreement shall be construed to
prevent the adoption or enforcement by any contracting party of measures
necessary to protect human, animal or plant life or health.’
The Doha declaration on TRIPs and public health was the first step towards
the restatement of such rights. It stated that ‘Each Member has the right
to grant compulsory licences and the freedom to determine the grounds upon
which such licences are granted’, and that ‘Each Member has the right to
determine what constitutes a national emergency or other circumstances of
extreme urgency, it being understood that public health crises, including
those relating to HIV/AIDS, tuberculosis, malaria and other epidemics, can
represent a national emergency or other circumstances of extreme urgency.’
However, the agreement did not specify conditions for parallel imports,
instead providing the now-infamous Paragraph 6, which ran as follows: ‘We
recognize that WTO Members with insufficient or no manufacturing
capacities in the pharmaceutical sector could face difficulties in making
effective use of compulsory licensing under the TRIPs Agreement. We
instruct the Council for TRIPs to find an expeditious solution to this
problem and to report to the General Council before the end of 2002.’
If the WTO establishment had been serious about fulfilling this promise,
the most straightforward way would have been for the exporting country to
make a limited exception from the patent privilege under Article 30. It is
noteworthy that so far the developed countries have succeeded in forcing
the discussion in the TRIPs Council away from the possibilities inherent
in Article 30 of the TRIPs agreement, which were discussed above. Instead,
they have focussed on Article 31, which is much more limited, constraining
and cumbersome.
The basic statement, which was finally cleared on 30 August, had actually
been formulated in 2001, but was held up by the US government on behalf of
its Big PhaRMA lobby (which incidentally had generously funded the Bush
and Republican election campaigns). The modified version that is now
cleared, has put in many more restrictions which drastically limit the
ability of importing countries to access cheaper generic substitutes, and
therefore contain the ability of such generic manufacturers to benefit
from economies of scale and emerge as real competitors of the large drug
companies.
All that the new statement does is waive the obligations of the exporting
country under Article 31(f) of the TRIPs agreement with respect to the
grant by it of a compulsory licence to a company, which was supposed to be
for the domestic market only. Export can be permitted to importing
countries that fulfil the following conditions.
First, the eligible importing member can only be a least developed
country or a developing country that does not have adequate facilities to
produce the drug in question. This importing country has to make a
notification to the TRIPs Council that:
- specifies the names and expected quantities of the products needed;
- confirms that the eligible importing Member in question, (other than a least developed country Member) has established that it has insufficient or no manufacturing capacities in the pharmaceutical sector for the products in question in one of various ways are which specified; and
- confirms that, where a pharmaceutical product is patented in its territory, it has granted or intends to grant a compulsory licence in accordance with Article 31 of the TRIPS Agreement and the provisions of this decision.
Importing countries
also have to ensure legal administrative means of preventing
re-exportation of any such drugs.
Similarly, the compulsory licence issued by the exporting member
has to contain the following conditions:
- only the amount necessary to meet the needs of the eligible importing Member(s) may be manufactured under the licence and the entirety of this production shall be exported to the Member(s) which has notified its needs to the Council for TRIPS;
- products produced under the licence shall be clearly identified as being produced under the system set out in this Decision through specific labelling or marking. Suppliers should distinguish such products through special packaging and/or special colouring/shaping of the products themselves, provided that such distinction is feasible and does not have a significant impact on price; and
- before shipment begins, the licensee shall post on a website information relating to the quantities being supplied to each destination and the distinguishing features of the products;
- (c) the exporting Member has to notify the TRIPS Council of the grant of the licence, including the conditions attached to it. The information provided has to include the name and address of the licensee, the products for which the licence has been granted, the quantities for which it has been granted, the countries to which the products are to be supplied and the duration of the licence, and the address of the relevant website.
It is amazing that the same developing countries which had been clamouring for a quick and fair resolution of the problem, have agreed to a decision that is so patently imbalanced in favour of large multinational patent holders, so restrictive and so unworkable for exporters and importers of generic drugs. The suspicion must be that this agreement, which had been held up for so long by the developed countries (especially the US) and the multinational drug lobby, has now been hammered down the throats of the unfortunate developing country negotiators, simply in order to show some results before the Cancun Meeting. If this is so, it certainly augurs badly for the outcome of other trade negotiations in Cancun.
© MACROSCAN
2003